Subdural hematoma after a car accident. Researchers from Arizona State University have developed a new tool to find out how a person can suffer brain injury from a car accident.
Auto accidents are the most common cause of emergency room visits, hospitalizations, and deaths associated with brain injuries among people ages 15 to 34, according to a 2013 report by the Centers for Disease Control and Prevention. At our office best car accident lawyers are ready to meet these situations 24/7 Contact Brad Nakase if you need seo services for lawyers Orange County.
We have already said that, in a normal person, the subdural space is practically virtual. One of the primary reasons is that the brain occupies almost the entire intracranial volume and, as we have seen in a previous lesson, there is a positive pressure, the intracranial pressure (ICP), which maintains this situation of pressure of the brain on the bone, “crushing”the subdural space.
But there are circumstances in the evolution of people that cause this not to happen, instead the brain moves away from the bone, increasing the subdural space. The most common are those that lead to brain atrophy, which involves a decrease in brain volume. Among those that stand out, among the pathological ones, chronic alcoholism or senile dementia due to Alzheimer’s disease. But, within natural evolution, with advanced age, there is a process of cerebral atrophy, not necessarily linked to loss of intellectual capacity, which can lead to the same situation of separation of the cerebral cortex from bone, with increased subdural space. .
It must be taken into account that, crossing this space, there are numerous veins that go from the cerebral cortex to the large drainage veins that are found inside the dura.
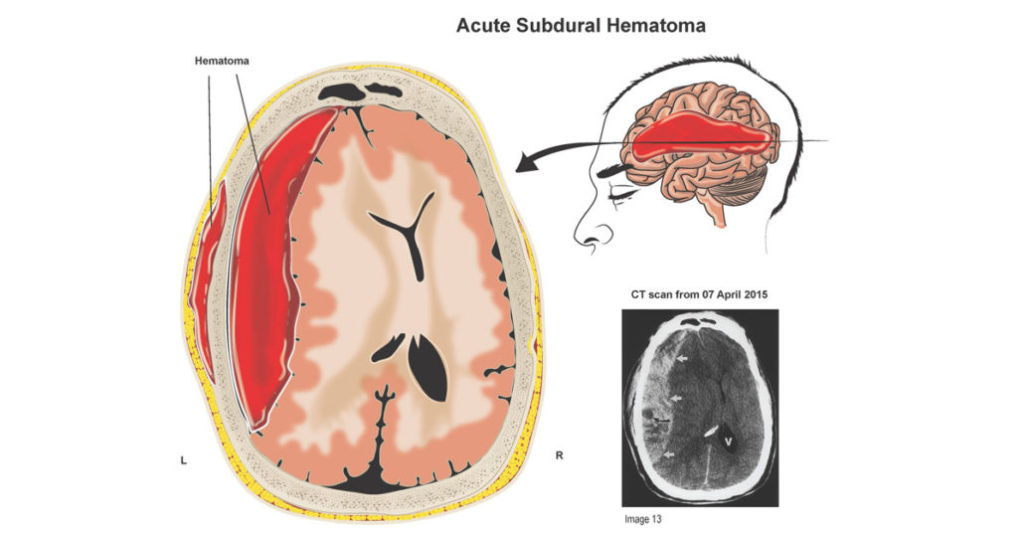
Now imagine a fortuitous blow to the head. Bone moves fast, but the brain has different inertia and moves at different speeds and times. This causes these drainage veins to tighten. If the blow is strong enough and the veins are already tense due to the distance between the cerebral cortex and bone, due to atrophy, a rupture of these veins can occur and consequent hemorrhage. The process of formation of the subdural hematoma begins.
The bleeding that occurs is small, since the veins that break are so. In addition, the blood remains in a space that can increase in size, so no brain injury or compression is caused. In other words, there is a period after that banal headache in which the patient feels nothing and continues his normal life.
The blood that has left the subdural space coagulates and subsequently suffers degradation, like any clot, with the intention of being reabsorbed. But this degradation process involves a breakdown of the large protein molecules. They are divided into several smaller ones. This facilitates reabsorption in any part of the body. But in the brain the situation is different.
This increase in molecules, by a physical law, increases the osmotic pressure in the liquid content of the cavity where the hematoma is. This increase in osmotic pressure attracts the water found in the adjacent spaces. Which translates into a progressive tendency to hematoma more liquid, but larger.
In this phase, the increase in volume may already initiate compression of the underlying brain. If the protein degradation process ends, it is possible that a positive evolution of reabsorption of the liquid content will begin, without squeal for the patient. But if the amount of blood is large enough and the process of protein degradation has not ended, maintaining a large osmotic pressure, the volume will continue to increase and a situation of certain intracranial hypertension will be reached.
To this situation it must be added that the expansion of the subdural space due to the increase in the volume of the hematic fluid can stretch and break new veins, which will produce new hemorrhages, thus generating a vicious circle of increased hematoma, rupture of new veins, increase in blood, increase in subdural hematic-protein content, etc., which ends in a very serious situation that can lead to the death of the patient.
The situation can be further complicated if the HSD becomes chronic. On the cerebral surface and below the dura, an increasingly dense membrane of vascular zed and active tissue forms, which aims to reabsorb the hematoma. This membrane can have the drawback that it can later perpetuate HSD in several ways: 1.- It secretes liquid into the HSD cavity. 2.- After evacuation of the blood content, it prevents the brain from expanding and “sticking” to the surface of the dura. 3.- Septations are formed, which divide the HSD cavity.
Although rare in adults, bilateral HSD can occur. In these cases, both subdural spaces are generally communicated, although they usually require bilateral evacuation intervention.
Leave a Reply